Diabetes – Fact versus Fiction
November is American Diabetes Month®. The vision of the American Diabetes Association is a “life free of diabetes and all of its burdens. Raising awareness of this ever growing disease is one of the main efforts behind the mission of the Association.”
Here are a few of the most recent statistics:
- Nearly 30 million children and adults in the United States have diabetes.
- Another 86 million Americans have prediabetes and are at risk of developing Type 2 diabetes.
- The American Diabetes Association estimates that the total national cost of diagnosed diabetes in the United States is $245 billion.
Nearly one in 10 Americans has diabetes. There are many myths that still remain. I hear them in my office all the time. Let’s set a few of these myths to rest and get the facts.
Myth: Everyone who is overweight develops diabetes.
Fact: Type 2 diabetes (which accounts for 90-95% of the cases) is much more common in people who are overweight. Excess weight IS the strongest known risk factor. Being overweight increases the chances of developing type 2 diabetes seven fold. Losing 7 to 10 percent of your current weight can cut your chances of developing type 2 diabetes in half. Losing any excess weight – and keeping it off – is the best defense against diabetes. However, keep in mind that other factors play a role as well: genetics, inactivity, age, and ethnicity. The key is to know your numbers and know your risk – prevention is key! (With type 1 diabetes, the body’s immune system attacks part of its own pancreas. Scientists are not sure why – more on Type 1 in a separate blog post).
Myth: If your fasting blood sugar is 100 to 125 (called prediabetes), you will develop type 2 diabetes.
Fact: Having prediabetes does not mean that you will develop diabetes. The risk is there and the key is to make lifestyle changes in order to prevent or delay it from progressing to diabetes. The scary fact is that many people come into my office with prediabetes and don’t know they have prediabetes. There are three reasons this could be the case. The first I call the “Charlie Brown” syndrome – it’s possible their doctor did tell them and all they heard was, “wah waaah wah wah”. The second reason is that their doctor told them they have prediabetes and they’re in denial and last but not least is the patient was never told by their doctor. 86 million people have prediabetes. This CAN be prevented or delayed from progressing to diabetes. Know your numbers.
Myth: People with diabetes need to eat special food.
Fact: The irony is that everyone should eat healthy food. It’s no different than what I recommend to anyone, diabetic or not. As people are faced with a diagnosis of diabetes they’re simply more pressed to make immediate changes. Healthy eating means having variety, balance, and moderation. I teach people to limit their intake of sodium, saturated (and trans) fat, added sugars and refined grains. I also teach people to place an emphasis on nutrient-dense foods, to increase their fiber intake, and begin to look at more whole foods and less processed (chemical enhanced) foods. The key is to implement one change at a time and then move on to the next. Healthy eating is a way of life, it’s not just a quick fix for a short period of time.
Myth: Eating sweets is off-limits for people with diabetes.
Fact: Variety, balance, and moderation. EVERYONE should limit their intake of sweets, not just people with diabetes. Indulging in too many sweets makes it more difficult for anyone to keep off unwanted pounds and leaves less room for the nutrient-rich foods the body needs. This is what I tell my patients: you know yourself, are you the kind of person who can have a piece of chocolate or are you the type of person that will have the whole chocolate bar? Having sweets lying around the house can only set you up to fail if you’re the type to eat the whole chocolate bar. The key is to allow for some of those moments with sweets and desserts, otherwise you’ll go overboard when you do see the desserts. In people with diabetes I always try and explain that it’s important to have good blood sugar control. Including these sugar-containing treats is possible with portion control and knowing their blood sugar levels – it’s called managing your diabetes. I teach them that desserts are a part of life (especially as the holidays are approaching), however, desserts are not the fuel source your body needs to operate at full-strength capacity. Always aim for the best fuel and keep the desserts in check.
Myth: Fruit is a healthy food. Therefore, it is okay to eat as much of it as you wish.
Fact: Yes fruit is a healthy food, but NO you cannot each as much of it as you wish. Fruit does contain fiber and lots of vitamins and minerals. However, fruit contains carbohydrates and therefore needs to be included as part of your meal plan, in a controlled amount. Since beginning work at the Diabetes Research Institute, this is one change I’ve made – I’ve decreased the amount of fruit I eat and started to increase the amount of non-starchy vegetables I’m consuming. Tough? Yes. Healthier for me? Absolutely! (p.s. Juicing, smoothie, and smoothie bowls as a trend needs to stop – the fiber is there but not functional and it tends to be a load of carbohydrates – EAT and CHEW your food.)
I’m always telling my patients to “know their numbers” Here’s a chart to help explain your numbers:
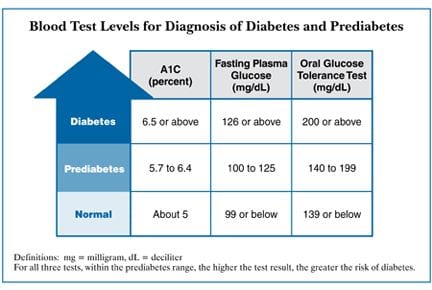
If you have your fasting blood sugar checked routinely for your doctor visits, the fasting blood sugar should be less than 100 mg/dL. If it is above 100 mg/dL this will be an indicator to have your A1c checked. The A1c is a blood test that runs an average over the last three months of your blood sugar level – so while your fasting blood sugar could’ve been high it doesn’t necessarily indicate your overall control. The A1c is the best test for verification. An A1c between 5.7-6.4% indicates prediabetes and an A1c at 6.5% and over is diabetes. This November, have yours tested so you can know your numbers. Knowing if the first part of prevention. Here are a few other tips to help reduce your risk:
Exercise moderately. Aim for 150 minutes of exercise/week. Inactivity promotes type 2 diabetes. Working your muscles more often and making them work harder improves their ability to use insulin and absorb glucose. This puts less stress on your insulin-making cells. Long hours of hot, sweaty exercise aren’t necessary to reap this benefit. Walking briskly for a half hour every day reduces the risk of developing type 2 diabetes by 30 percent. Limit the time you spend sitting at work, at home, or in between.
Tune Up Your Diet – Making a few dietary changes can have a big impact on the risk of type 2 diabetes.
- Choose whole grains and whole grain products over highly processed carbohydrates. Whole grains don’t have a magical nutrient that fights diabetes and improves health. It’s the entire package – elements intact and working together – that’s important. The bran and fiber in whole grains make it more difficult for digestive enzymes to break down the starches into glucose. This leads to lower, slower increases in blood sugar and insulin, and a lower glycemic index. As a result, they stress the body’s insulin-making machinery less, and may help prevent type 2 diabetes. Whole grains are also rich in essential vitamins, minerals, and phytochemicals that may help reduce the risk of diabetes.
- Skip the sugary drinks and choose water. When it comes to diabetes, sweet beverages seem to be a double-whammy. Their high-fructose corn syrup and other sugars increase the demand for insulin and have a high glycemic load. The sugar you sip may add flab more than the sugar you chew. Liquid calories don’t seem to lead to satiety and the reduction in subsequent food intake that you might have with solid calories. It’s easy to take in a large amount so easily. Think your drink.
- Include heart-healthy plant-based fats. The types of fats in your diet can also affect the development of diabetes. Healthy fats, such as the polyunsaturated fats found in liquid vegetable oils, nuts, and seeds can help ward off type 2 diabetes. Trans fats do just the opposite. These unhealthy fats are found in many margarines, packaged baked goods, fried foods in fast-food restaurants, and any product that lists “partially hydrogenated vegetable oil” on the label.
- If You Smoke, Try To Quit. Smokers are roughly 50 percent more likely to develop diabetes than nonsmokers, and heavy smokers have an even higher risk.
- Alcohol Now and Then May Help. A growing body of evidence links moderate alcohol consumption with reduced risk of heart disease. The same may be true for type 2 diabetes. Moderate amounts of alcohol – up to a drink a day for women, up to two drinks a day for men – increases the efficiency of insulin at getting glucose inside cells. If you already drink alcohol, the key is to keep your consumption in the moderate range, as higher amounts of alcohol could increase diabetes risk. If you don’t drink alcohol, there’s no need to start – you can get the same benefits by losing weight, exercising, and changing your eating patterns.
The bottom line to prevent type 2 diabetes: Keep your weight – and especially your waist – under control, and spend more time on your feet than on your seat.